Your Journey Starts Here,
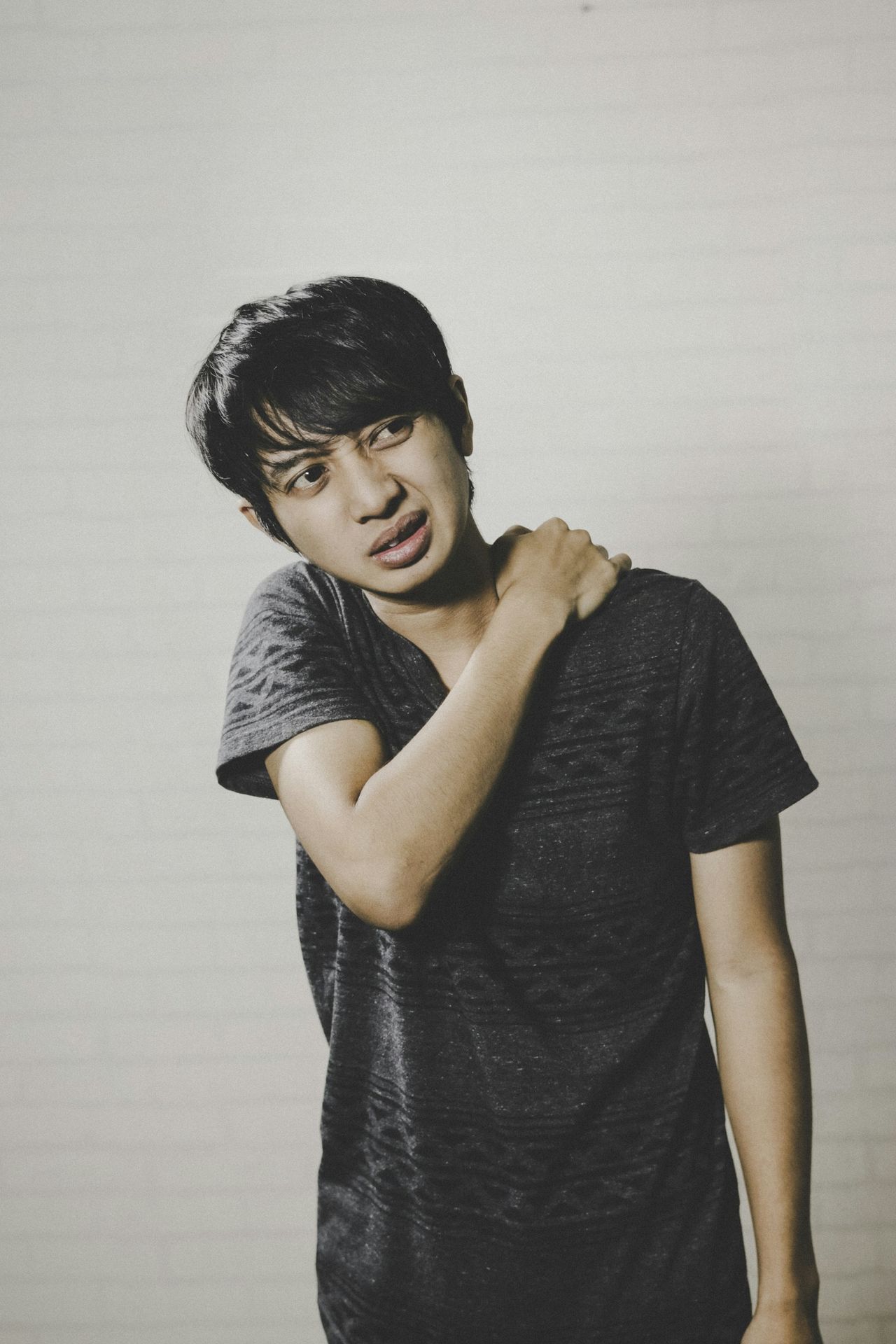
Comprehensive Shoulder Pain Treatment and Therapy
Shoulder pain can significantly impact your daily life, whether it originates within the shoulder joint itself or from the surrounding muscles, ligaments, and tendons. At Beyond Care Physical Therapy & Wellness, our skilled physical therapists are experts in identifying the source of your shoulder pain and providing effective, personalized treatment to restore mobility and function. Remember, if your shoulder pain is accompanied by breathing difficulties or chest tightness, seek immediate medical attention, as it could be a sign of a heart attack.
How Physical Therapy Can Help Your Shoulder Pain
Our physical therapists are highly trained specialists dedicated to evaluating and treating movement dysfunctions. With expertise in a variety of shoulder conditions, they work to enhance your mobility and overall quality of life.
By employing personalized treatment plans and advanced techniques, our therapists focus on alleviating pain and restoring function. Their goal is to empower you to regain strength and confidence in your daily activities.
Comprehensive Evaluation and Assessment
We thoroughly assess your shoulder pain, movement patterns, and contributing factors.
Personalized Treatment Plans for Your Needs
Our expert team creates individualized plans to restore mobility, reduce pain, and improve overall shoulder function.

Conditions We Successfully Treat
We have extensive experience in treating a variety of shoulder conditions, including:
Shoulder pain and instability
Addressing weakness and instability.
Rotator cuff injuries and tears
Rehabilitating strains and tears.
Tendonitis and impingement syndromes
Managing inflammation and compression.
Post-surgical rehabilitation
Guiding recovery after shoulder surgery.
Frozen shoulder (Adhesive Capsulitis)
Restoring range of motion.
AC joint separations
Rehabilitating injuries to the acromioclavicular joint.
Sports-related injuries
Specialized care for athletes.

Adhesive Capsulitis (Frozen Shoulder)
Adhesive capsulitis, commonly referred to as frozen shoulder, is a condition characterized by inflammation and stiffness of the shoulder's joint capsule. This condition results in significant pain and a marked reduction in the range of motion, making everyday activities challenging for those affected.
The exact cause of adhesive capsulitis remains elusive; however, several contributing factors have been identified. Conditions such as minor trauma, diabetes, and prolonged immobilization of the shoulder can increase the risk of developing this painful disorder, highlighting the importance of early intervention and appropriate management strategies.
Stages and Recovery
Frozen shoulder, also known as adhesive capsulitis, is characterized by a gradual onset of shoulder stiffness and pain, progressing through three distinct stages: freezing, frozen, and thawing. In the freezing stage, individuals experience increasing pain and a gradual loss of shoulder mobility, which can last several months.
This is followed by the frozen stage, where the pain may diminish, but significant stiffness persists, making it difficult to perform everyday activities.
Finally, in the thawing stage, shoulder mobility begins to improve, and the pain gradually subsides, leading to a return to normal function.
Although frozen shoulder is a self-limiting condition, the recovery process can be lengthy, often taking up to two years or more for complete resolution During this time, physical therapy and pain management strategies can play a crucial role in facilitating recovery and improving quality of life.
Our Physical Therapy Approach
Our comprehensive physical therapy approach for frozen shoulder combines targeted exercises, manual therapy, and personalized care to restore mobility and alleviate pain.
Patient education to understand the condition
Targeted stretching to improve flexibility.
Joint mobilization to restore movement.
Structured home exercise programs for continued progress
Rotator Cuff Tear/Injury
Rotator cuff tears are a significant concern in both younger and older populations, often arising from acute injuries in active individuals or from the natural wear and tear of tendons in older adults. These tears can lead to debilitating shoulder pain, particularly during overhead activities, and may result in noticeable weakness and difficulty in arm elevation.
The impact of a rotator cuff tear extends beyond physical limitations, affecting daily activities and overall quality of life. Early diagnosis and appropriate management are crucial to alleviate symptoms and restore function, highlighting the importance of understanding the underlying causes and manifestations of this common shoulder injury.
Diagnosis and Treatment
Diagnosis often involves imaging like MRI. Treatment varies by age and severity.
Younger patients may require surgical repair
Older individuals often manage with activity modification
Anti-inflammatory medications for symptom relief
Physical therapy to regain strength and mobility.
Cortisone injections may be considered
Surgery if conservative treatments fail

Shoulder Tendonitis and Impingement
Tendonitis is a condition characterized by the inflammation of the shoulder tendons, leading to symptoms such as pain, warmth, redness, tenderness, and a noticeable reduction in shoulder function. This inflammation can significantly impact daily activities, making it difficult for individuals to perform tasks that require shoulder movement.
Rotator cuff tendonitis, a specific type of shoulder tendonitis, often arises from factors such as overuse, fatigue, trauma, or the natural degeneration of the tendons over time. Athletes and individuals engaged in repetitive overhead activities are particularly susceptible, as the constant strain can lead to chronic inflammation and discomfort in the shoulder region.
Understanding Impingement
Impingement occurs when rotator cuff tendons are compressed beneath the acromion, aggravated by repetitive overhead movements, heavy lifting, or sleeping on the affected shoulder. X-rays may reveal bone spurs or a hooked acromion.
Treatment Options
Rest to reduce strain.
Physical therapy to improve strength and mobility.
Anti-inflammatory medications (e.g., ibuprofen).
Cortisone injection for symptom relief in some cases.

Labral Tear
The labrum is a crucial structure in the shoulder joint, functioning as a cartilage ring that deepens the socket and enhances the stability of the upper arm bone. By providing a more secure fit, it allows for a greater range of motion while minimizing the risk of dislocation.
Labral tears can occur due to various factors, including acute trauma, chronic shoulder instability, or repetitive overhead activities, such as those performed in sports or certain occupations. These injuries can lead to pain, decreased mobility, and a feeling of instability in the shoulder, often necessitating medical evaluation and treatment.
Symptoms and Diagnosis
Symptoms include painful clicking, locking, or popping sensations, and sometimes instability. Diagnosis is typically by MRI, though tears can be challenging to detect. A SLAP tear is a specific type that may involve the biceps tendon.
Treatment Approach
Treatment options for a labral tear include physical therapy, anti-inflammatory medications, corticosteroid injections, and surgical repair, depending on the severity of the injury.
Often involves arthroscopic repair.
Treatment for a labral tear often involves arthroscopic repair, a minimally invasive procedure that allows surgeons to fix the damaged cartilage through small incisions. This approach reduces recovery time and alleviates pain, while physical therapy may be recommended afterward to strengthen the joint and restore function.
Specialized treatment for SLAP tears
Specialized treatment for SLAP tears focuses on a combination of physical therapy, surgical intervention, and rehabilitation to restore shoulder stability and function.

Shoulder Instability
Shoulder instability is a condition characterized by the abnormal movement of the shoulder joint, which can result in either a complete dislocation or a partial dislocation known as subluxation. This instability often arises from trauma, repetitive overhead activities, or inherent ligamentous laxity, leading to significant pain and functional limitations.
The most frequent type of shoulder dislocation is anterior dislocation, where the humeral head shifts forward out of the glenoid cavity. However, shoulder instability can also manifest as posterior dislocation or multidirectional instability, each requiring tailored treatment approaches to restore joint stability and function.
Causes and Symptoms
Risk is highest with an abducted and externally rotated arm (e.g., fall on outstretched hand). Symptoms can range from immediate noticeable dislocation to a sensation of slipping with or without pain, or "apprehension" with certain arm movements.
Immediate and Long-Term Care
Sudden dislocation requires immediate medical evaluation for nerve/blood vessel damage.
Pain relievers, muscle relaxants, and ice help manage discomfort.
For recurring instability, activity modification, physical therapy, or surgical stabilization may be considered.
Emergency room physicians can often manually reposition the joint.
Physical therapy typically starts 2-3 weeks post-dislocation for strengthening and stability.

Posterior Shoulder Dislocation
Posterior dislocations, characterized by the arm moving backward out of the shoulder socket, are relatively uncommon, accounting for only about 4% of all shoulder dislocations. This type of injury can be particularly challenging to diagnose due to its subtle presentation and may often be overlooked in clinical assessments.
In contrast, posterior subluxation is gaining recognition, especially among athletes in sports such as tennis and baseball, where repetitive overhead motions can predispose individuals to this condition. As awareness grows, it becomes crucial for sports professionals and medical practitioners to identify and manage these injuries effectively to prevent long-term complications and ensure optimal recovery for athletes.
Emergency and Rehabilitation
"Treatment options for Posterior Tibial Tendon Dysfunction (PTTD) include conservative measures like orthotics and physical therapy, as well as surgical interventions for advanced cases."
A sudden posterior dislocation is a medical emergency; immediate evaluation is crucial.
Emergency room physicians can usually manually reposition the joint.
Pain relievers, muscle relaxants, and ice manage discomfort.
Physical therapy typically begins 2-3 weeks post-dislocation to strengthen supporting muscles.

Multidirectional Instability
Ligamentous laxity is a condition characterized by the excessive looseness of the ligaments that support the shoulder joint, which can result in instability. This instability often manifests as pain and weakness, particularly when the shoulder partially dislocates, or subluxes, in various directions, including forward, backward, or downward.
During a clinical examination, a positive "sulcus sign" can be a key indicator of this condition, as it reveals the presence of inferior shoulder instability. This sign is elicited by pulling down on the arm while the patient is relaxed, and the resulting indentation or "sulcus" beneath the acromion suggests that the ligaments are not adequately stabilizing the joint.
Treatment Approach
Treatment options for multidirectional shoulder instability include physical therapy, activity modification, and, in persistent cases, surgical interventions such as capsular shift or labral repair.
Most patients respond well to physical therapy focusing on strengthening shoulder muscles and improving stability.
Surgery is rarely recommended due to the challenges of stabilizing the shoulder in all directions.
Acromioclavicular Separation
An AC (acromioclavicular) separation is a common injury that often results from a direct impact or fall onto the shoulder, leading to significant pain and swelling in the affected area. Patients may notice a visible deformity, as the collarbone can appear to protrude, indicating a disruption in the joint where the collarbone meets the shoulder blade.
The severity of an AC separation can vary, with symptoms ranging from mild discomfort to severe pain that limits mobility. Treatment options depend on the extent of the injury, with some cases requiring conservative management through rest and physical therapy, while more severe separations may necessitate surgical intervention to restore proper alignment and function.
Treatment Approach
Treatment options for acromioclavicular separation include conservative management with rest and physical therapy, as well as surgical intervention for more severe cases.
Generally includes rest, ice, and pain management with anti-inflammatory medication.
Physical therapy to restore motion and strength.
Considering Elbow Pain?
If you're dealing with elbow discomfort, tightness, or restricted movement, our skilled physical therapists offer specialized care for numerous elbow issues. Whether it's lateral epicondylitis or medial epicondylitis, we develop customized treatment strategies aimed at helping you regain your range of motion and experience enduring relief.
Take the First Step Towards Shoulder Pain Relief. Book Your Appointment Today!
Don't let shoulder pain limit your life. Our experienced physical therapists are here to help you on your journey to recovery.